Blog 3 of the 4 Part Series: Why I Want a COVID-19 mRNA Vaccine (and why you should too).
This is the third of four blog posts where I share what I have learned as a Tallahassee pediatrician doing my own research, and why I am excited to receive a COVID-19 vaccine:
- Last Sunday – How vaccines use our immune system to protect us against viruses, bacteria, and even cancer.
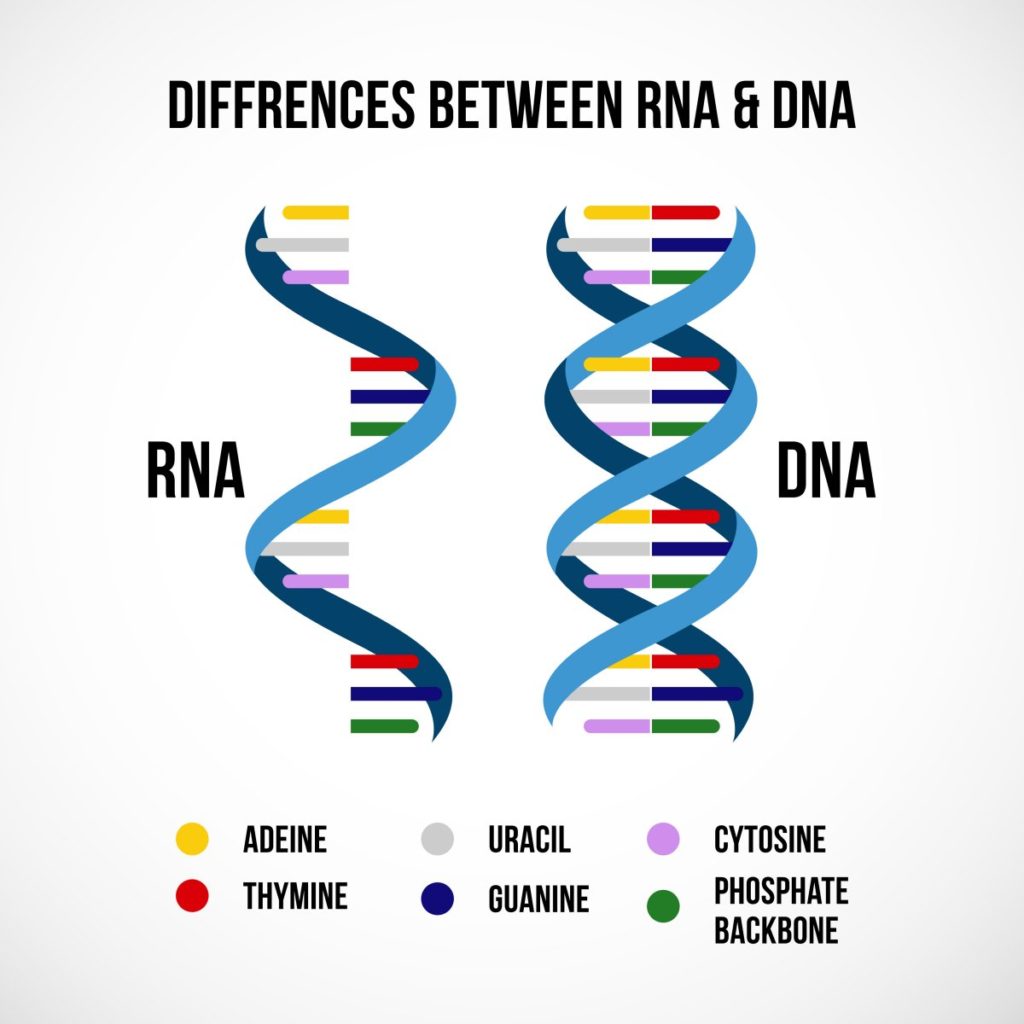
- Last Wednesday – How mRNA and DNA vaccines are different than traditional vaccines.
- Today – mRNA and DNA vaccine safety in animals and humans.
- This Wednesday December the 16th – Post Covid-19 Syndrome
The History of mRNA and DNA Vaccines
Starting around 1990, scientists were first able to inject genetic material (mRNA or DNA) into animal muscle AMD get the muscle cells to produce a protein based on this genetic material. This laid the foundation for mRNA and DNA vaccines, which stimulate the muscle cells near the injection to produce the antigen for the vaccine. So far, the biggest challenge with DNA and mRNA vaccines has not been safety but getting them to work. Scientists have continued to tweak the antigen code and the adjuvant effect of the DNA and mRNA. They have also discovered better ways of getting the mRNA or DNA into the cells.
DNA and RNA Vaccines in Humans and Animals
Though the new COVID-19 mRNA and DNA vaccines will be the first fully licensed vaccines for humans, there have been DNA vaccines licensed for animals since 2002. This includes vaccines for fish, dogs, cats, horses, and chickens. None of these licensed vaccines for animals have had to be pulled from the market for safety or efficacy concerns.

mRNA and DNA Vaccines were already in Human Clinical Trials
Starting 10 years before the COVID-19 pandemic, mRNA vaccines had started entering human clinical trials. This includes vaccines against influenza, rabies, cancer, Mono, and Zika virus. In fact, Moderna had already completed a successful Phase 1 Clinical Trial for an mRNA influenza vaccine in 2017. Most of the mRNA vaccines in trials have been safe and effective, but just like traditional antigen plus adjuvant vaccines, some mRNA vaccines were not effective and some had too strong of an immune response. But after a decade of conducting mRNA vaccine trials on thousands of human lives, results have been so good and promising that research and interest has continued to grow.
COVID mRNA Vaccines are 90-95% Effective, in Studies of Over 50,000 People
I am so impressed with reports of 90 to 95% effectiveness. Yes, the Phase 3 Clinical Trials are just finishing, and we only have about 9 months of safety data in humans, but 95% efficacy is awesome! First, many vaccines and medications get to Phase 3 trials just to find out that they do not really work. Second, this is exceeding the CDC’s goal for 70% effectiveness (the seasonal flu vaccine is only 40 to 60% effective every year). 95% Efficacy means that if you give 100 people the COVID-19 mRNA vaccine, and then expose them all to COVID-19, only 5 out of the 100 would contract COVID-19!
COVID mRNA Vaccines have been Safe
So far, COVID mRNA vaccines have been safe. About 1/3rd of people who received the Moderna or Pfizer/BioNTech mRNA vaccines had a reaction. Normally a little redness or swelling at the injection site or mild aches or fatigue. About 2% (2 out of every 100 shots) of study participants had a “grade 3” reaction, which means that the fever, body aches, fatigue, or swelling was severe enough to keep the person from doing his or her normal activities for a day or two. There were no life-threatening “grade 4” reactions in with either mRNA vaccine trial. This is similar to what people experience after a Tdap (tetanus-diptheria-whooping cough) booster vaccine.
What Other Adverse (aka Bad) Reactions were Scientists Worried About?
Some scientists were worried about too strong of an immune response from the adjuvant part of the mRNA. This could have led to high fevers, inflammation, damage of vital organs, or too much swelling at the injection site Thankfully, even though the mRNA immune response has been strong (which is good because it stimulates the body to build antibodies), it has not been dangerously strong. Again, the experience is similar to receiving a Tdap vaccine.
Second, scientists were worried about “Vaccine Enhanced Disease,” where the vaccine makes the real infection worse rather than protecting against the infection. There were some animal vaccine studies of the 2002 SARS Coronavirus (which is similar to COVID-19), in which the experimental vaccine made the SARS infection worse, so scientists were appropriately nervous about VED occurring with COVID-19 vaccination. Thankfully this has not happened. Even when vaccinated people get COVID-19, the COVID-19 infection has been less severe, instead of more severe. More great news!
Third, DNA and mRNA are genetic material. There is a theoretical concern that a DNA or mRNA vaccine could permanently insert foreign genetic material into our DNA, leading to health problems. In the decades of DNA and mRNA vaccine experimentation, this has never happened in animal or human studies (but it could make a good movie).
In conclusion, the COVID-19 mRNA vaccines appear to be very safe and very effective, despite the rapid development and challenges of making a new vaccine. Thankfully, mRNA and DNA vaccines had been in development for decades and were ready to be produced when the COVID-19 Pandemic hit.
I hope after reading this (long) blog, you are encouraged and excited about how our country can overcome this horrible illness. Post with any questions, and read my next blog covering Post Covid-19 Syndrome.